Contact number: 020 7806 4060
What is Thumb Joint Replacement Surgery?
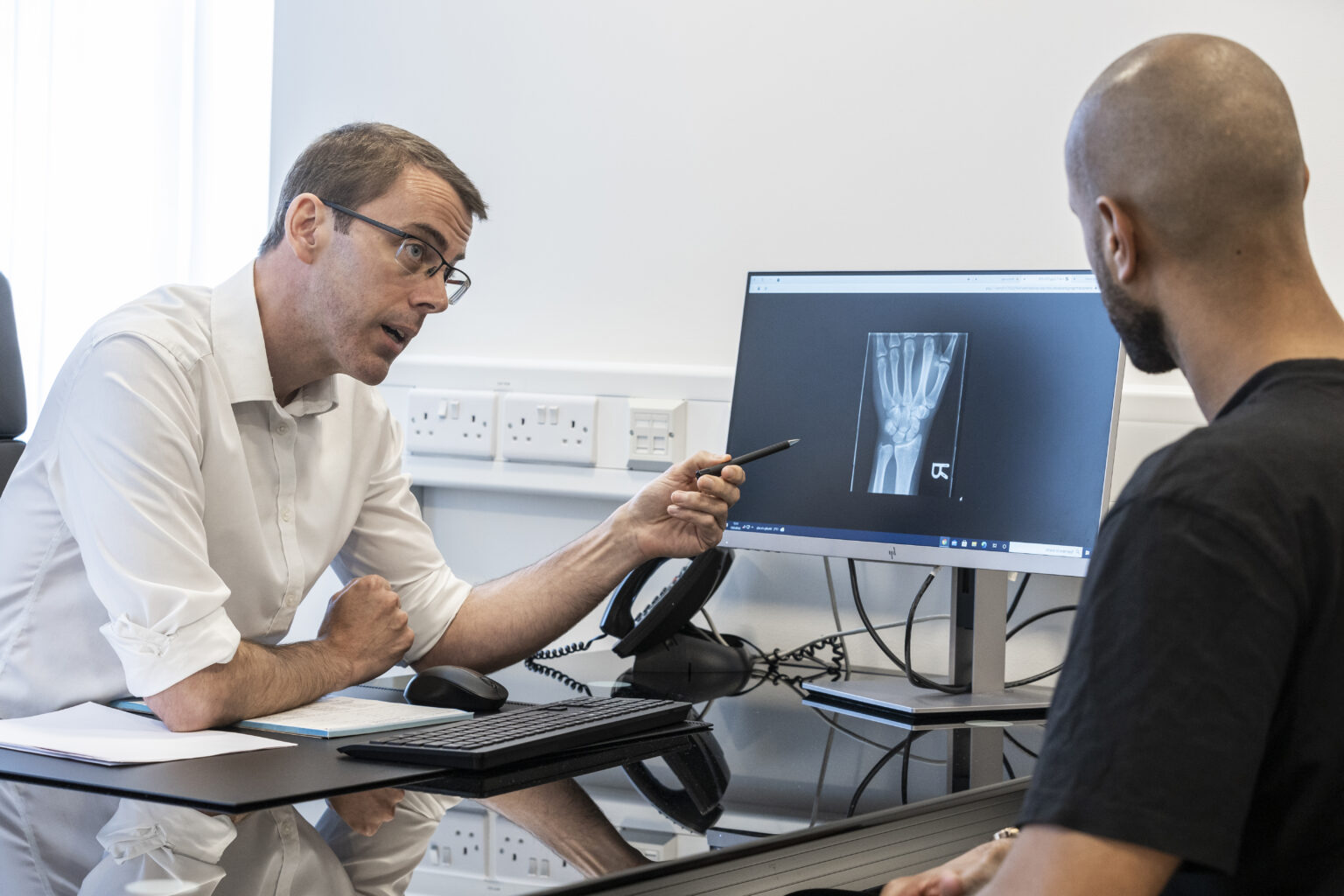
Thumb joint replacement involves removing the damaged joint surfaces and replacing them with an artificial implant, typically made from metal, plastic, or ceramic. The procedure is most commonly performed on the basal joint at the base of the thumb, which is frequently affected by osteoarthritis.
This surgery is recommended for patients with chronic pain, reduced grip strength, or limited thumb mobility that hasn’t improved with non-surgical treatments like splints, injections, or physiotherapy.
Located in St John’s Wood (NW8), our hospital provides thumb joint replacement surgery in modern facilities designed for optimal care and recovery.
Thumb Joint Replacement Surgery at St John & St Elizabeth Hospital
At St John & St Elizabeth Hospital, we offer personalised treatment plans for thumb arthritis and joint damage. Our expert hand surgeons focus on effective pain relief and long-term restoration of thumb function.
Why choose us for thumb joint replacement surgery?
- Specialist Hand Surgeons: Our consultants have extensive experience in joint replacement and hand surgeries.
- Advanced Techniques: We use the latest surgical methods and high-quality implants for lasting results.
- Modern Facilities: Our hospital is equipped with advanced equipment, enabling our specialists to perform accurate diagnoses and deliver highly effective treatments tailored to each patient’s needs.
- Accessible Location: Conveniently based in NW8, we serve patients from Hampstead (NW3), Kilburn (NW6), and across London.
We are committed to helping you regain a pain-free, functional thumb through expert care and support.
How to pay for your treatment
If you’re… paying for yourself
Did you know you don’t need private medical insurance to come to St John & St Elizabeth Hospital? As a self-pay patient, you can access safe, outstanding quality health care at times to suit you.
For scans and tests, as well as to see most consultants, you’ll still need to be referred by a medical professional like your GP, but as a self-pay patient, the process is more straightforward. You won’t need authorisation from an insurance provider, and you’ll have greater choice of consultant and appointment times.
If you’re… insured
St John & St Elizabeth Hospital is approved by all major medical insurance companies. If you have a personal private health insurance policy, or your company provide it for you, you can use it to pay for your care from your initial consultation through to treatment, surgery and aftercare such as physiotherapy. Not all private health insurance plans cover the same things. It’s very important to check exactly what you are covered for with your insurance provider.
Frequently Asked Questions About Thumb Joint Replacement Surgery
St John & St Elizabeth Hospital is located in St John’s Wood (NW8), a well-connected area of North West London. We are conveniently accessible for patients from Hampstead (NW3), Kilburn (NW6), and beyond.
By Tube:
- St John’s Wood station (Jubilee Line) is just a 5-minute walk from the hospital.
- Finchley Road (NW3) and Kilburn stations (NW6) on the Jubilee Line provide excellent connections.
- By Bus:
Wellington Road: Routes 13, 46, 82, and 113 stop near St John’s Wood Underground Station, just a short walk from the hospital.
Circus Road: Routes 46 and 187 stop close to the hospital’s Circus Road entrance.
Abbey Road: Routes 139 and 189 stop near the junction where Grove End Road becomes Abbey Road, providing easy access.
Major Roads:
If you’re travelling from NW3 or NW6, major routes such as Finchley Road or Kilburn High Road offer a direct approach to the hospital.
Our hospital ensures convenient access for patients across London, particularly those in NW8, NW3, and NW6 postcodes.
What are the symptoms of base of thumb arthritis?
Osteoarthritis leaves the thumb joint unable to move as smoothly as it should. This causes pain, swelling and restriction of movement. It is not possible to predict how osteoarthritis will develop and progress in each individual.
Your symptoms may vary for no clear reason – you may have good and bad days. However, some patients do notice that certain activities make their symptoms worse.
Common symptoms include:
- Pain – This tends to feel worse when you move your thumb or at the end of the day.
- Stiffness – Your thumb may feel stiff after rest, but this usually wears off with movement. The joint may also creak or crunch when you move it.
- Restricted movement – Your thumb may not move as freely or as much as normal. You may find everyday tasks difficult, such as texting, opening jars or turning a key.
- Appearance – In advanced cases, there may be a bump at the base of the thumb and the middle thumb joint may bend back, looking like a zigzag. The muscles around your joint may look thin and your thumb may swell.
Self-Help
- Consider using heat (hot water bottle or heat pack) and taking a painkiller before going to bed.
- Consider adapting your work environment.
- Eat a well-balanced, healthy diet. Some people find getting additional nutrients from food supplements can be helpful. Important vitamins and minerals to consider when you have arthritis are calcium, vitamin D and iron. Turmeric, glucosamine, selenium, and vitamin C are also potentially helpful supplements, but don’t help everyone.
Hand Therapy
A hand therapist can provide you with a home exercise programme to help reduce joint stiffness and improve thumb movement. When you have arthritis, it is important to keep your joints moving and improve the strength of the muscles which control the thumb.
Your therapist may also educate you on activity modification, joint protection, adaptive equipment, and splinting.
Our hospital has an excellent hand therapy service which can support you.
Pain Management
Paracetamol, anti-inflammatory medications (such as aspirin and ibuprofen) or anti-inflammatory gels may help reduce pain. This should always be discussed with a doctor or pharmacist who can give you appropriate advice.
Joint injections
If you are still struggling with pain after trying other non-surgical interventions, a steroid injection may provide temporary relief.
It’s important to note that:
- Injections are not always successful in relieving pain, and the length of time for which they work varies from patient to patient. They can take 2-3 weeks to take effect.
- Injections carry a risk of infection, increased pain, and skin changes.
Your consultant will discuss whether an injection is an appropriate treatment for you.
The procedure typically takes 45 to 90 minutes, depending on the complexity of the joint damage and the surgical technique used.
The surgery will start with a cut in the skin near the thumb so your surgeon can access the joint. The surgeon will then remove any damaged cartilage and bone from your thumb and wrist and replace it with an artificial implant made from metal and plastic. Your surgeon will close your incision with stitches and cover it with bandages. The procedure usually takes one hour and most patients can return home the same day.
Thumb joint replacement surgery is performed under local or general anaesthesia, ensuring you won’t feel pain during the procedure. Some discomfort and swelling are normal afterwards but can be managed with medication and rest.
Recovery involves rest, hand exercises, and physiotherapy to restore strength and mobility. Most patients can return to light activities within a few weeks, while full recovery may take up to three months
Recovery time varies from patient to patient, but most people can expect some discomfort and swelling in their hand for the first few weeks after surgery.
Two weeks after surgery, you will need to have a check-up with your consultant where your stitches will be removed. You will then need to wear a splint or a thumb cast for several weeks to protect the new joint and aid healing.
Specialist hand therapy is often recommended after surgery to help strengthen the hand and improve movement. Our hand therapy service can support patients with their recovery.
Recovery from a thumb joint replacement typically takes several months to a year, with a gradual return to normal activities and optimal hand function. Your exact timeline will vary depending on individual factors and adherence to rehabilitation.
Thumb joint replacement is recommended for patients with severe arthritis or joint damage that has caused chronic pain, reduced grip strength, or limited thumb movement and has not responded to non-surgical treatments.
When you are ready to leave after surgery, you will need someone to collect you from hospital as you will not be able to drive.
Medically reviewed by Mr Alistair Hunter - MA MBBS MSc FRCS (Tr&Orth) FHEA Dip Hand Surg on 13/11/2023